The goal of Restore Health is to provide an alternative to the traditional approaches to preventing the onset of chronic diseases
The goal of Restore Health is to provide an alternative to the traditional approaches to preventing the onset of chronic diseases

The next generation of EHRs will focus more on the doctor, making their jobs easier

MGMA Senior Vice President of Government Affairs Anders Gilberg gives a glimpse at what’s happening on the Hill

With lives on the line, medicine has to be far more careful with advancements

Mobility should be the basis of anything given to doctors

McClellan, a former CMS and FDA leader, discusses how to transform health care in the wake of the COVID-19 pandemic, and the role for primary care.

New technology plays a key role in getting physicians what they need to treat patients

Balancing rapid access needed by physicians while protecting patient privacy is a difficult task

Evidence-based insights are going to change health care in the future

What you need to know about making telehealth pay off now and in the future.

There are financial, legal and operational considerations physicians must consider as they deal with COVID-19 and flu season.

New practice models give some hope to physicians looking to make it on their own

The march toward value-based care is inevitable

Many practices are facing down a huge revenue shortfall from the pandemic's shut down. But there are ways to recoup your losses and grow your practice.

Data is the key to showing payers the value physicians bring to the table

Physicians in independent practice need to embrace change

States have changed restrictions on nurse practitioners

Access points for primary care are rapidly increasing
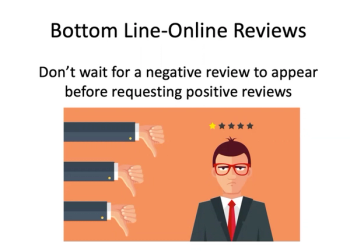
Tips to promote your online reputation through good patient reviews.

Fee-for-service medicine will remain for many years to come.

Practices should guarantee as much revenue as possible upfront

Patient demand for telemedicine will remain after the COVID-19 pandemic, and as a result more payers will reimburse for it

Flexibility and the ability to adapt to unforeseen events are key to good financial forecasting

This flu season, physicians must stress importance of vaccinations — and find creative ways to provide them.

Practices should take advantage of federal and state programs

Practices need to regularly evaluate their revenue and expenses

With the right infrastructure, they can make a case to payers that they are a valuable asset.

David Zetter, founder of Zetter HealthCare LLC, says practices can ease patients’ safety concerns by informing them of all the safety measures the practice has put in place.

While independent medical practices face significant challenges, they are an important part of the health care market and need to be protected.

Practices need to follow CDC guidelines