
Healthcare spending grew at 4.6 percent in 2018 to $3.6 trillion, which was faster than 2017.

Healthcare spending grew at 4.6 percent in 2018 to $3.6 trillion, which was faster than 2017.

Patients are unwilling to wait for an appointment with their physician and will delay care due to difficult scheduling.

This year's third-place finisher.

What physicians need to know when reviewing contracts

How artificial intelligence can boost surgery center operations and revenue cycle management.

A new study from the Kaiser Family Foundation shows a small percentage of Medicare beneficiaries in private Medicare Advantage plans changed their plans during the 2016 open enrollment period.

By embracing two-way texting as a communication channel for patient engagement, practices can achieve significant improvements throughout their operations.

Real estate is the second highest expense behind payroll for most healthcare practices.

Firing patients for no-shows and non-adherence is a difficult decision, and there are important factors to consider.

A review of 11 different studies found that physicians with a positive screening for depression were highly likely to report medical errors.

A study of life expectancy and mortality rates in the U.S. found it has risen since 1959, but the last three years have seen a decrease.

EHRs can handle all clinical aspects of the revenue cycle with ease, but they lack visibility into the back end of the revenue cycle.

Sentara Hospitals agreed to take corrective action for an April 2017 HIPAA violation

Centers in five metropolitan areas will offer wellness services and Medicare plan resources after they open in January 2020

Physicians understand the connection between mental and physical health, yet many don’t feel equipped to address patients’ behavioral health problems.

Malpractice suits require some unique defenses.

Protect your reputation from disgruntled patients.

The second-place entry in this year's Physician Writing Contest

If your practice is like most other practices, then one area where you could use some work is billing and collections. Here are six resolutions that can improve your billing and collections in 2020.

Don’t leave the management and growth of your practice up to chance. Now is the right time to think about what you want to achieve in 2020. Here’s how to prepare.
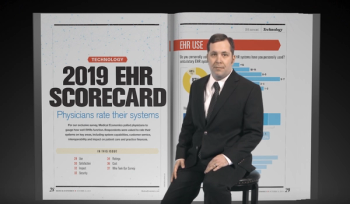
Medical Economics sat down with Andrew Pecora, MD, to discuss why EHR data sharing is so difficult, and potential solutions to this complex issue

What physicians need to know about the rise of home health technology.

The hospitals claim HHS Secretary Alex M. Azar II illegally extended Medicare payment reductions which were meant to expire in 2017.

The ability to maximize collections and profitability is vital for medical practices.
Time to brush up on some particularly festive ICD-10 codes

Google Health says the Project Nightingale partnership is aimed at creating and testing a new EHR interface.

Kentucky hospital will pay millions to settle allegations it submitted false claims to Medicare.

Summary: Buying medical malpractice insurance independently requires substantial investigation into the specifics.

Three red-flags a doctor is about to quit.

Sutter Health and the Sacramento Cardiovascular Surgeons Medical Group agree to pay more than $46 million to settle allegations rising from claims made to Medicare