Practice Finance
Latest News
Latest Videos

Shorts
Podcasts
CME Content
More News

When health care providers can’t keep up with the cost of modernizing their equipment, patients lose access to the latest, most effective tools for care.

Private equity investment will spur additional oversight, but investors and the community could benefit
Practices may boast high clean claim rates yet still bleed revenue; shifting to a first-pass payment focus, smarter workflows and tech-driven visibility can transform reimbursement performance and cash flow.
How to get paid for continuing relationships with patients who have complex, serious conditions.

Loren Adler, fellow and associate director at the Brookings Institution’s Center on Health Policy, joins the show to discuss how payer ownership is reshaping primary care and what it means for independent physicians.

Navigating compliance and capital in a rapidly evolving health care M&A market

Many private medical practices across the country are facing increasing challenges as a result of many factors, most notably lower reimbursement and higher overall practice expenses, which together result in lower physician take-home compensation. Is it time to look at new options?
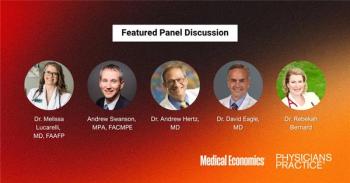
A panel of physicians, practice leaders and health care experts unpacks what true independence looks like in 2025 and breaks down how practices can strengthen their footing for the years ahead.

Clarissa Riggins, chief product officer at Experian Health, joins the show to talk why denied claims are increasing and how AI can help practices prevent revenue loss.

A decade of federal initiatives strengthened care coordination, engagement and clinical quality in primary care, but fee-for-service incentives kept spending high.

How reliable point of sale systems can enhance patient experience and operational efficiency in small medical practices, ensuring seamless service.

WalletHub’s latest CPI analysis reveals which metro areas are seeing prices rise fastest.

Practices using remote physiologic monitoring expanded care access without cutting visits for other patients.
Medical Economics and Physicians Practice hosted a roundtable on the future of independence practice.

Hidden fees, staff turnover and opaque contracts are quietly eating into your practice’s bottom line.

What doctors think about AI solutions for RCM

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

With denials cutting deeper into practice revenue, physicians are turning to AI-driven tools to catch errors before submission, automate appeals and reduce administrative burnout.

A new survey from Smarter Technologies and MedCity News shows hospitals and practices waiting months for payment, battling costly billing software and turning to AI for relief.