News
Article
ACP recommends pharmacologic treatments for Type 2 diabetes
Author(s):
Reducing risks of all-cause mortality is a goal with new treatment options.
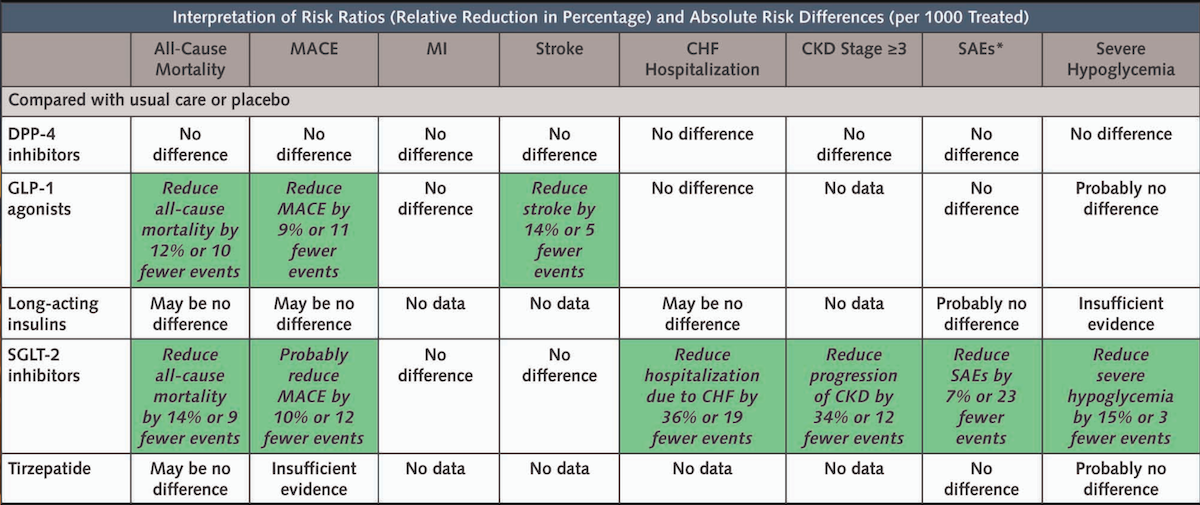
This chart was published as part of “Newer Pharmacologic Treatments in Adults With Type 2 Diabetes: A Clinical Guideline From the American College of Physicians,” updating the College's 2017 treatment guidelines.
© American College of Physicians
Newer pharmacologic treatments are recommended for the armamentarium to treat Type 2 diabetes, according to the American College of Physicians (ACP).
Physicians and other clinicians treating patients with T2d and inadequate glycemic control should consider adding a sodium-glucose cotransporter-2 (SGLT-2) inhibitor or glucagon-like peptide-1 (GLP-1) agonist to metformin and lifestyle interventions.
“As additional pharmacological treatments become available for the treatment of Type 2 diabetes, it’s critical for us to examine their effectiveness, the harms and benefits as well as costs in order to provide the best treatment for our patients,” ACP Guidelines Committee Chair Carolyn J. Crandall, MD, MS, MACP, Chair, said in the College’s announcement. “Adding a second medication to metformin for patients with inadequate glycemic control may provide additional benefits but the added benefit on important clinical outcomes may be minimal in relation to the high cost, particularly for the more expensive, newer medications.”
The SGLT-2 inhibitor aims to reduce risk of all-cause mortality, major adverse cardiovascular events, progression of chronic kidney disease, and hospitalization due to congestive heart failure. The GLP-1 agonist could reduce the risk of all-cause mortality, major cardiovascular events, and stroke, according to ACP.
ACP recommended against adding a dipeptidyl peptidase-4 (DPP-4) inhibitor to metformin and lifestyle modifications in adults with T2d and inadequate glycemic control. The DPP-4 does not reduce morbidity or all-cause mortality, based on high-certainty evidence, according to ACP.
ACP used its GRADE approach, short for Grading of Recommendations, Assessment, Development and Evaluation, to evaluate high-priority outcomes:
- All-cause mortality
- Major adverse cardiovascular events
- Myocardial infarction
- Stroke
- Hospitalization for congestive heart failure
- Progression of chronic kidney disease
- Serious adverse events
- Severe hypoglycemia
The updated guideline focuses on clinical benefit outcomes. It did not look at effects of treatment for glycemic control, a common treatment goal, because it is established that all included treatments can improve glycemic control in adults with T2d. There was not sufficient data to use GRADE to rate weight loss, measured by a percentage of participants achieving at least 10% total body weight loss, although it was a prioritized outcome.
The latest guideline updates the 2017 clinical recommendations and is based on the best available evidence for effectiveness, comparative benefits and harms, consideration of patients’ values and preferences, and costs, said an announcement from ACP.
“ACP guidelines emphasize shared decision-making, recognizing that each patient's needs and circumstances are unique,” the College’s announcement said. “ACP encourages physicians to consider individual patient characteristics like age, comorbidities, and personal preferences when discussing a treatment plan for Type 2 diabetes.
“SGLT-2s and GLP-1s are costly, but lower cost options (like sulfonylureas) were inferior in reducing all-cause mortality and morbidity,” the ACP announcement said, adding “there are currently no generic formulations for GLP-1s and SGLT-2.”
The College published “Newer Pharmacologic Treatments in Adults With Type 2 Diabetes: A Clinical Guideline From the American College of Physicians,” on April 19 in Annals of Internal Medicine.
Newsletter
Stay informed and empowered with Medical Economics enewsletter, delivering expert insights, financial strategies, practice management tips and technology trends — tailored for today’s physicians.