ADA and AACE Guidelines for Type 2 Diabetes Mellitus
Episodes in this series

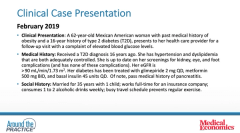
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: That’s a great transition. From what you just mentioned, Dr Busch, what do we do from a guideline standpoint? We have the ADA [American Diabetes Association] Standards of Medical Care in Diabetes, and we have the AACE [American Association of Clinical Endocrinology] Clinical Practice Guidelines. What is recommended for optimal glycemic control in patients with type 2 diabetes at diagnosis and obviously as they progress? We’ve learned from Dr Brunton—and we’ve known this—that this is a progressive disease. The therapies we’re going to need are going to change, and you may be right with what you might need in the beginning vs later therapy. If you could, walk us through where we are from a guideline standpoint.
Robert Busch, MD: We’ve evolved from the “keep a little sugar in the urine” approach from many years ago, to the “lower is better” approach today. With UKPDS [United Kingdom Prospective Diabetes Study] in type 2 diabetes or with BCCT [Beyond Conventional Cancer Therapies] and type 1 diabetes, you felt that the lower your microvascular disease, the lower your A1C [glycated hemoglobin] was. We’re now in a different world where we have diabetes drugs that can lower macrovascular disease. Both guidelines have evolved in a way that say you not only want to get A1C down, but it’s how you’re getting A1C down as well. Avoiding hypoglycemia is very important.
We have a tantalizing array of drugs. When Stephen and I started practicing, we just had sulfonylurea therapy, and we now have drugs that work in each of those defects.
Stephen A. Brunton, MD, FAAFP: When I started, we only had leeches, so you’ve come a long way since then.
Robert Busch, MD: And ways to diagnose the diabetes. You may have had patients urinate on the wall and looked if the ants crawled up the wall. You may have done double void urines. With our younger colleagues, they do finger sticks and continual monitoring.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: I’m glad Diana and I didn’t have to worry about that.
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: Yeah. I even think finger sticks are archaic now.
Robert Busch, MD: Right. That’s exactly right, and we had double void urines. We were adjusting the mpH [metabolic pH] in the morning based on the double void at dinnertime. Things are totally different, which is the fun we all have going to work. We can always do 1 better than we used to be.
Getting A1C down would be important, whether it’s the AACE guidelines of 6.5% or the ADA guidelines below 7%, as well as how you do it. AACE was always ahead of the game; it had a batting order of the drugs. You didn’t want to cause hypoglycemia, and you wanted to use drugs that have excellent efficacy after metformin, and the AACE guidelines were a GLP1 and then SGLT2. If you use those, you used what Stephen was talking about with the ominous octet.
Metformin worked at the liver with no hypoglycemia weight loss. GLP1 lowered glucagon at alpha cell, increased insulin at glucose-dependent weight, delayed stomach emptying, and lowered appetites. You had many things covered with weight loss and no hypoglycemia. That’s SGLT2 making you urinating out sugar with weight loss and no hypoglycemia.
Those are the big 3 classes used by a lot of our colleagues. However, a lot of our colleagues still use other drug therapies. There’s still too much use of sulfonylurea therapy, whether it’s because of the cost or habit, especially with the doughnut hole, where patients can’t afford some of the drugs, especially patients using Medicare. Both the ADA and AACE evolved in a way that, once we had all these drugs that we knew had cardiac benefit, we looked at the patient. If they’ve had previous ASCVD [atherosclerotic cardiovascular disease], then you have to give them a heart-smart drug, like an SGLT2 or GLP1. The ADA went further: If you had kidney disease or heart failure, then the SGLT2 should be the priority over the GLP1. We have these great drugs prior to giving insulin, but as I’m sure we’ll be discussing, over time, many patients require insulin as well.
Stephen A. Brunton, MD, FAAFP: Those points are very important. We’ve gone from being very glucose-centric in our approach to really looking at outcomes. We didn’t have that data until after the FDA required them, in 2008, for us to do cardiovascular outcome trials. We’re in a renaissance, if you will, in terms of our management. We have so many more agents that we can use to tailor our therapy to the physiology as well as looking at outcomes as our focus and not just getting the glucose down.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: That’s helpful. In years past, we would have potentially been having a discussion, and I would have been asking Dr Brunton about how the ADA does things this way and the guidelines are written like this. I would have been saying to Dr Busch that AACE is suggesting this, and there would be a lot of confusion. I would say that, in recent years, there’s been a lot of alignment, and have you sensed that there’s less confusion now among ATPs [authorized treating physicians] on where certain drugs fall and what 1 guideline is saying vs the other? I would love the primary care and the endocrine perspectives there from a guideline standpoint. Is there less confusion or more confusion? Where do you see that?
Stephen A. Brunton, MD, FAAFP: From a primary care perspective, we probably looked to the ADA more than AACE. A lot of my colleagues are not aware of AACE guidelines. However, to your point, they’re much more synchronous than they used to be. Though there may be a slight difference in terms of all A1C targets, in terms of therapeutic approaches, the cardiovascular-acting trials have directed how we approach the management in a more logical manner.
Robert Busch, MD: Despite those guidelines and what Stephen has just talked about, when a patient is referred into us for primary care, we still see much too much use of DPP4 rather than GLP1, and there is still a lot of sulfonylurea use. The sulfonylurea, I can understand because it’s inexpensive and done out of habit, although we don’t use any if we don’t have to. The DPP4s, without any cardiovascular benefit, are still overused a lot. Most of my colleagues and the diabetology colleagues I respect a lot are using GLP1 rather than the DPP4. It is not so much from the AACE guidelines. It’s for the other benefits with weight loss and cardiovascular benefit vs weight neutral and no cardiovascular benefit. As we all know, DPP4 is easy to use: open mouth, insert pill. You don’t have to worry about nausea, injection, or anything like that.
Stephen A. Brunton, MD, FAAFP: It’s also economics. I’ve worked with a restrictive formulary, and the only things we had available besides metformin was sulfonylureas and leeches. We had to go that way. The DPP4s are easy to use, as we said, but they also may have wider coverage than some of the other agents. If you are trying to get the glucose down, you might go to that as a second or third option just to get the glucose down. You then may have some more barriers to getting more logical agents. That may be what’s driving primary care’s usage of those agents.
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: I want to add that there is a lot of therapeutic inertia. If you have someone who’s already progressed to multiple daily injections, even though they would benefit from the cardiovascular outcomes of GLP1 agonists and SGLT2 inhibitors, people sometimes don’t think of that. In endocrinology, we get a lot of referrals of people who haven’t been on the therapies that we know can help them, and we’re often even adding them to their multiple daily injections. We’re adding them because we know they have good cardiovascular outcomes.
Stephen A. Brunton, MD, FAAFP: To your point, Diana, that therapeutic inertia is a critical issue. The ADA is working on a task force with that. Part of the thing is that we delay up to 7 years or longer before we add another agent despite the fact the A1C is rising. It’s that the pressures in practice are such that it’s easy to wait another 3 months for the patient who says, “Just give me more time.” We need to recognize that, if we treat aggressively and get patients to go earlier, there’s a legacy effect. We can decrease the impact and the development of some of these other problems the longer they’re on. There is a lot that we need to do, and there is a lot of pressure on us in practice. The data are showing that there’s a real benefit to taking that role.
Newsletter
Stay informed and empowered with Medical Economics enewsletter, delivering expert insights, financial strategies, practice management tips and technology trends — tailored for today’s physicians.