Article
Coding Cues
Well-woman exams
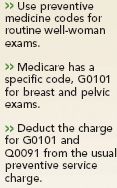
Although practices generally have one fee for a well-woman exam, the visit typically encompasses three portions: a general preventive examination that's age- and gender-appropriate; a gynecological exam, including a breast and pelvic exam; and a Pap smear.
Use 99385-99397
For instance, if you see a new patient, you'll report one of three codes:
For an established patient, you should report one of these codes:
There's a catch, though: Medicare doesn't cover routine annual preventive exams. So when you do a well-woman exam for a Medicare beneficiary, you should attach modifier –GY (item or service statutorily excluded or does not meet the definition of any Medicare benefit) to the preventive care code. The modifier indicates that the service isn't covered and allows Medicare to correctly state the amount the patient owes on the EOB.
And don't try to code a preventive exam with a new or established patient office visit E&M code (99201-99215) in order to get the service covered. Doing so can be construed as coding for reimbursement instead of based on correct coding guidelines; that's fraud, says Vicky V. O'Neil, a certified coder and owner of The Hazlett Group in St. Louis. You should always select the E&M code based on the visit's purpose.
You can report 99205-99215 to Medicare in addition to a screening Pap test and a screening breast and pelvic exam if you document a separate and distinct E&M service and you attach modifier –25 to the E&M code. For example, you can use an E&M code if you manage the patient's diabetes in addition to performing the Pap and pelvic exam.
Coding different services
You don't usually report routine breast and pelvic exams separately. Many private payers include them in 99385-99397. And CPT contains no codes for reporting these services.
But Medicare does offer a specific code for breast and pelvic exams. When you perform this service for Medicare beneficiaries, you should assign G0101 (cervical or vaginal cancer screening; pelvic and clinical breast exam).





