Article
Coding Cues
Chronic conditions
Here's what you need to know about properly coding chronic conditions.
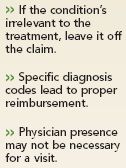
Is the condition relevant?
For example, a patient with high cholesterol (272.0, pure hypercholesterolemia) arrives with a closed fracture of a rib (807.01, closed fracture of one rib). He isn't on any medication now. You treat the fracture without manipulation (21800, closed treatment of rib fracture, uncomplicated, each). In this case, you should code only the broken rib. Because the patient's cholesterol level wasn't medically relevant and you didn't address it, you shouldn't include code 272.0.
On the other hand, if the patient's cholesterol had affected your treatment options-say you had had to consider the condition when prescribing medication-then you could have reported the high cholesterol along with the fracture.
For instance, say a diabetic patient presents with an acute extrinsic asthma attack (493.02). The diabetes may put the patient at increased risk of infection and affect your ability to choose steroids as an anti-inflammatory. In this case, the chronic condition-diabetes (250.xx)-does affect your treatment options, so you should code for it.
Know documentation rules
While some payers and experts say you can choose which documentation guidelines to use for E&M services-either the 1995 guidelines or the ones from 1997-other payers want you to use the 1997 guidelines when it comes to "status of chronic conditions." This is the case even if you use the 1995 guidelines for other services. That's because the 1997 documentation guidelines require greater documentation of chronic conditions for an extended history of present illness (HPI). The 1995 guidelines don't mention chronic conditions as a history element, says Hvizdash. Check with your payer to learn their requirements.
Say you specifically question a patient about her diabetes (250.xx), pulmonary edema (514, pulmonary congestion and hypostasis), and high blood pressure (401.x, essential hypertension). All are chronic conditions and, under the 1997 guidelines, will require documentation as part of the history taking.
When the nurse does the exam
Many chronic conditions involve frequent checkups that may not always require your presence in the exam room. How do you code these visits?
For example, say a patient presents for a blood sugar log review for potential medication adjustment for Type II uncontrolled diabetes. The log review is performed by a nurse in accordance with the patient's plan of care. You'd report 99211 (office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician. Usually the presenting problems(s) are minimal. Typically, five minutes are spent performing or supervising these services) for the visit, Falbo says. The diabetes code should be 250.02 (diabetes mellitus without mention of complication; Type II or unspecified type, uncontrolled). Be sure that the documentation shows the medically necessary reason for performing the blood sugar log review.
Or say a patient presents for a blood pressure check to assess whether the medication you recently started him on is working. The BP is taken by a nurse following the plan of care you established for hypertension.





