Article
Coding Consult
Answers to your questions about ECG interpretation; after-hours codes; venom injections
ECG interpretation Q How can I get paid for interpretation of an inpatient ECG?
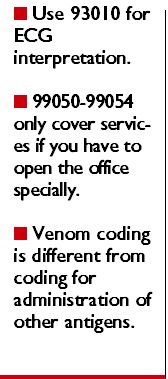
Your best bet to ensure the carrier pays for 93010 is to document that you interpreted the ECG's printout and didn't simply look at the ECG report. Why? The ECG technical component (93005, . . . tracing only, without interpretation and report) includes the machine's report. Carriers want to see that you performed an interpretation if you submit 93010. The hospital will bill for 93005.
A Although you should use 99050-99054 as add-ons to other E&M codes such as 99201-99215, you can report them only when you actually have to open the office to see a patient, not when you're running behind and you stay late.
For example, a patient calls you on Saturday, when your office is generally closed, needing treatment for an acute problem. You believe the problem can't wait until Monday, yet it isn't serious enough to send the patient to the ED. You see him in your office. This carries expenses, but ultimately saves the insurance company and the patient from paying ED costs.
To get paid for that visit in addition to the appropriate E&M code, report one of the following:
Venom injections Q We're having a problem getting reimbursed for allergy injections for stinging insect venoms. Should we bill the same for these injections as for the other allergy immunotherapy injections?
A You're facing a common problem, and there's an easy explanation for your predicament.
Coding for stinging insect venom is slightly different from coding for administration of other antigens. First, you need to understand the unique codes for insect venoms and insect antigen doses. When you bill for venoms, the number of insects and the number of doses are important:
This is different from the allergen antigens, in which the number of antigens in the vial is not relevant. CPT holds that these codes do not include coverage for the antigen administration.
If you prepare five doses of an antigen containing three stinging insect venoms, the coding would be 95147 times five, and 95117 (professional services for allergen immunotherapy . . . ; two or more injections) for the administration of each dose at each encounter. Whether the doses come from the same multiple-dose vial or a series of vials doesn't matter.

This information provided by The Coding Institute. For a free sample issue or information on how to subscribe to any of 29 specialty-specific coding newsletters, please contact The Coding Institute, 2272 Airport Road South, Naples, FL 34112; phone 800-508-2582; fax 800-508-2592; or visit http://www.codinginstitute.com





