Article
Coding Consult
Diabetes screening.
Expect your Medicare carrier to pay in the neighborhood of $5 to $17 for the tests, according to the Clinical Laboratory Fee Schedule. You can't bill patients for the screening tests, and the Medicare deductible and coinsurance or copayment don't apply.
Coverage guidelines
If the patient has none of these risk factors, you can still be paid if you document at least two of the following:
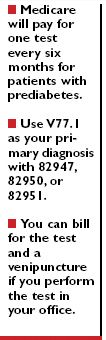
You may bill one test every six months for patients with prediabetes. CMS defines this as a condition of abnormal glucose metabolism diagnosed from a previous fasting glucose level of 100-125 mg/dL or a two-hour post glucose challenge of 140-199 mg/dL. Prediabetes includes impaired fasting glucose and impaired glucose tolerance.
For patients not diagnosed with prediabetes, you can bill only one test every 12 months.
Don't report screening codes to Medicare for a patient whom a physician has already diagnosed with diabetes (250.xx), because the patient obviously doesn't require screening.
You should also avoid these codes if the patient shows symptoms of uncontrolled diabetes, such as excessive thirst (783.5, polydipsia) or frequent urination (788.41, urinary frequency). Medicare already covers those conditions for diagnostic diabetes testing.
Use modifiers
To screen a Medicare patient for diabetes, use one of these codes:
Submit only one code per patient since Medicare pays for only one test. Whichever code you use, record V77.1 (special screening for diabetes mellitus) as your primary diagnosis code, according to CMS.
The three Medicare-approved diabetes screening tests carry a "waived status." That means if your office has obtained the appropriate CLIA certification, you can perform the tests in the office. Be sure you attach modifier –QW (CLIA-waived test) to the codes (for example, 82950–QW).





