- Revenue Cycle Management
- COVID-19
- Reimbursement
- Diabetes Awareness Month
- Risk Management
- Patient Retention
- Staffing
- Medical Economics® 100th Anniversary
- Coding and documentation
- Business of Endocrinology
- Telehealth
- Physicians Financial News
- Cybersecurity
- Cardiovascular Clinical Consult
- Locum Tenens, brought to you by LocumLife®
- Weight Management
- Business of Women's Health
- Practice Efficiency
- Finance and Wealth
- EHRs
- Remote Patient Monitoring
- Sponsored Webinars
- Medical Technology
- Billing and collections
- Acute Pain Management
- Exclusive Content
- Value-based Care
- Business of Pediatrics
- Concierge Medicine 2.0 by Castle Connolly Private Health Partners
- Practice Growth
- Concierge Medicine
- Business of Cardiology
- Implementing the Topcon Ocular Telehealth Platform
- Malpractice
- Influenza
- Sexual Health
- Chronic Conditions
- Technology
- Legal and Policy
- Money
- Opinion
- Vaccines
- Practice Management
- Patient Relations
- Careers
CMS introduces new ACO Primary Care Flex model
Five-year test starts in 2025 to promote innovative, proactive approaches to care.
The U.S. Centers for Medicare & Medicaid Services published this graphic to explain the new ACO Primary Care Flex Model, a five-year test model that will begin in 2025.
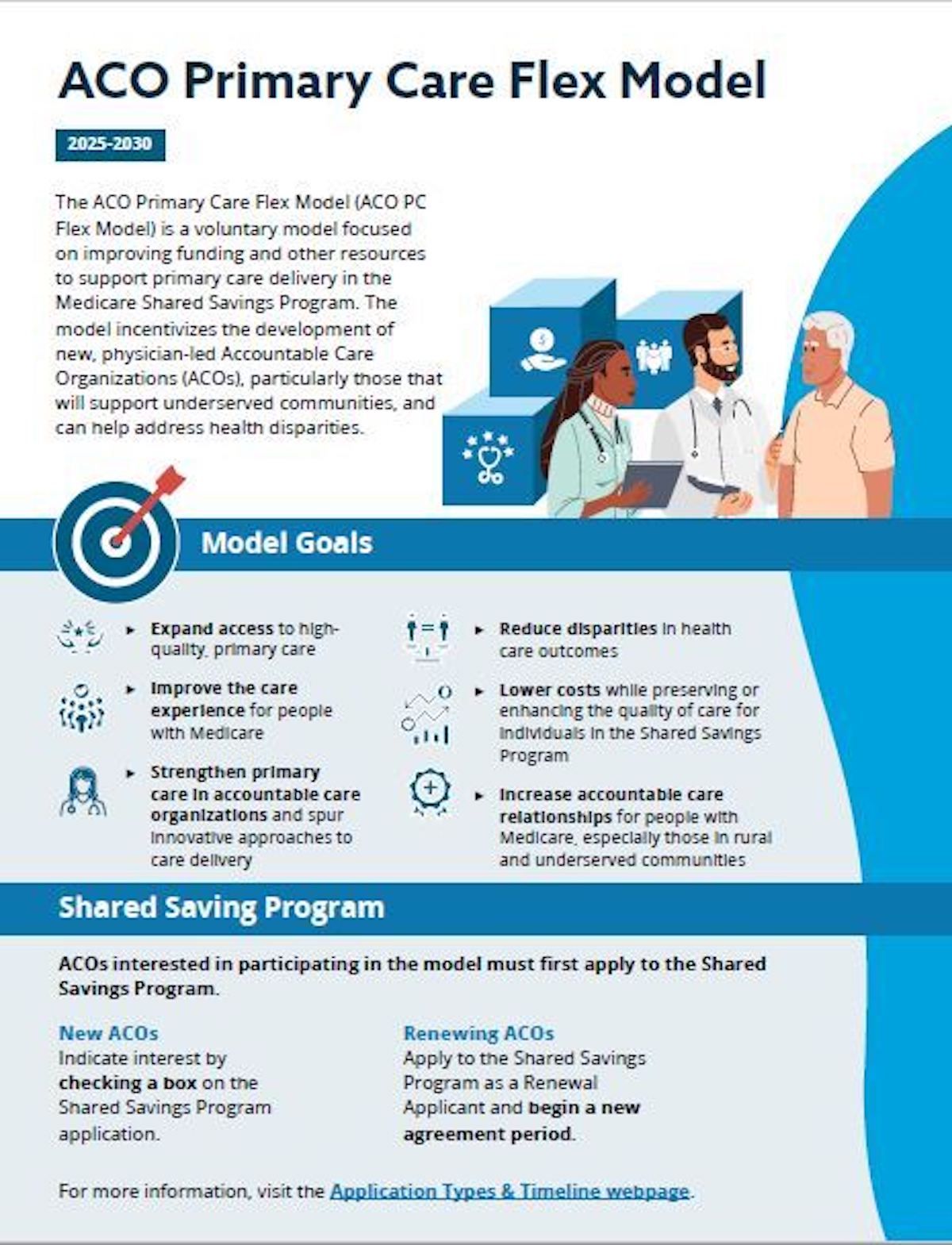
A new accountable care organization (ACO) model aims to enhance primary care while moving toward the goal of having Medicare beneficiaries in ACOs by 2030.
The ACO Primary Care Flex Model, also known as ACO PC Flex Model, was introduced this month with a focus on primary care delivery in the Medicare Shared Savings Program (MSSP). It was part of discussion in a wide-ranging quarterly conference call with leaders of the Centers for Medicare & Medicaid Services (CMS) held April 30.
ACO PC Flex will start Jan. 1, 2025, is a five-year test model. It will serve as an example of using the MSSP “as a chassis for innovation,” said Elizabeth Fowler, PhD, JD, CMS deputy administrator and director of the Center for Medicare and Medicaid Innovation.
“The flexible payment design will empower participating ACOs and their primary care providers to use more innovative, team-based, person-centered and proactive approaches to care,” said the official description.
That translates to two new payment mechanisms for ACOs, Fowler said.
A one-time advance MSSP payment can cover costs associated with forming an ACO if that’s relevant, and pay for administrative costs for implementing the model’s required activities, Fowler said.
A second monthly Prospective Primary Care Payment is intended to shift payment away from fee-for-service, visit-based payment to increase the predictability of primary care funding for low-revenue ACOs, she said.
“In contrast to previously tested models, the prospective payment rate is not based on historical spending estimates,” Fowler said. “Instead, it's based on a county's average primary care spending before social and clinical risk factors are applied. This will help reduce entrenched disparities in primary care investment and utilization by giving all beneficiaries in the country access to the same level of care regardless of which ACO serves them in a county.
“The model includes policies designed to ensure that the funds flow to primary care providers and are used specifically to support primary care,” she added.
The monthly payment is designed to support advanced comprehensive primary care, which coordinates the majority of a patient’s routine physical and mental health needs. Primary care physicians and other clinicians are encouraged to use more innovative, team-based, person-centered and proactive approaches to care, Fowler said.
“Proactive team-based approaches can include behavioral health integration, care management and patient navigation services,” she said. “We're really excited for what this means for primary care and I think it's a really important model that will do a lot of good for a lot of beneficiaries.”
The model is based on a recommendation in the National Academies of Sciences, Engineering and Medicine report, “Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care.” The report suggested paying primary care through ACOs to better support team-based care and provider infrastructure.
CMS currently has additional information and program goals posted online.
Drug price negotiations
CMS Deputy Director and Center for Medicare Administrator Meena Seshamani, MD, PhD, said the organization is leading implementation of the Medicare drug price negotiations allowed under the federal Inflation Reduction Act.
“We are actively engaged in negotiations with the manufacturers of all of the drugs that were selected for negotiation this year,” she said. “And we're continuing to learn from this first cycle of negotiations to prepare for the next cycle.”
Her comments came a day after another federal judge tossed a lawsuit filed by Bristol Myers Squibb and Johnson & Johnson to block the negotiations. Reuters reported U.S. District Judge Zahid Quraishi in Trenton, New Jersey, became the fourth federal judge to uphold the price negotiations as Big Pharma contends it is an illegal taking of their property.
Prescription drug price cap
CMS also will launch a “robust education” campaign on the new prescription drug out-of-pocket price cap of $2,000 beginning in 2025. Seniors also will be allowed to spread out drug costs through monthly payments, Seshamani said.
“This will be a relief to many seniors who are currently spending thousands of dollars a year on their drugs and removing this burden will provide meaningful financial relief, and we are actively working to engage diverse groups on spreading the word about the program,” she said.
MA payments
Participants included CMS Administrator Chiquita Brooks-LaSure; Sara Vitolo, deputy director for the Center for Medicaid and CHIP Services; Dora Hughes, MD, MPH, acting chief medical officer and acting director of the Center for Clinical Standards and Quality; and Eden Tesfaye, senior adviser to Brooks-LaSure.
The Medicare Physician Fee Schedule was not part of discussion. However, Seshamani noted the Medicare Advantage and Part D rate announcement is projected to result in a 3.7% average increase in payments to Medicare Advantage (MA) plans year over year. The federal government will pay more than $16 billion more in 2025 to MA plans than in 2024, she said.
The MA payments ensure “that MA plans are paid adequately to provide stability for enrollees,” Seshamani said.
