- Revenue Cycle Management
- COVID-19
- Reimbursement
- Diabetes Awareness Month
- Risk Management
- Patient Retention
- Staffing
- Medical Economics® 100th Anniversary
- Coding and documentation
- Business of Endocrinology
- Telehealth
- Physicians Financial News
- Cybersecurity
- Cardiovascular Clinical Consult
- Locum Tenens, brought to you by LocumLife®
- Weight Management
- Business of Women's Health
- Practice Efficiency
- Finance and Wealth
- EHRs
- Remote Patient Monitoring
- Sponsored Webinars
- Medical Technology
- Billing and collections
- Acute Pain Management
- Exclusive Content
- Value-based Care
- Business of Pediatrics
- Concierge Medicine 2.0 by Castle Connolly Private Health Partners
- Practice Growth
- Concierge Medicine
- Business of Cardiology
- Implementing the Topcon Ocular Telehealth Platform
- Malpractice
- Influenza
- Sexual Health
- Chronic Conditions
- Technology
- Legal and Policy
- Money
- Opinion
- Vaccines
- Practice Management
- Patient Relations
- Careers
Health care price transparency, competition on the agenda for House
Primary care at the table as Health Subcommittee hears from CMS chief, industry advocates on the flow of money.
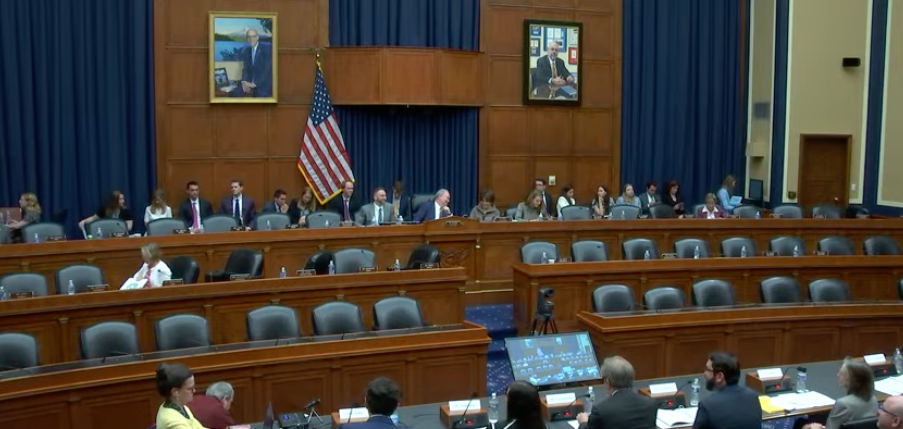
The U.S. House Energy & Commerce Subcommittee on Health convened April 26, 2023, for “Lowering Unaffordable Costs: Legislative Solutions to Increase Transparency and Competition in Health Care.” This screen shot was taken from the Subcommittee's online hearing that day.
The United States spent $4.3 trillion on health care in 2021, a larger percentage of the nation’s gross domestic product than the rest of the developed world.
So, who gets that money?
It depends who you ask, and Congress is asking.
The U.S. House Energy & Commerce Subcommittee on Health convened April 26, 2023, for “Lowering Unaffordable Costs: Legislative Solutions to Increase Transparency and Competition in Health Care.” It was the second part of a bipartisan hearing that began March 28 to discuss “the need to improve price transparency in health care as well as improve competition amongst payers and providers of health care to help lower costs for patients,” according to the hearing memorandum. It listed 17 bills that could affect health care policy and finances.
Get primary care involved
Primary care was at the table when six witnesses testified in the second panel of the day.
Primary care network Aledade Inc. estimated its accountable care organizations (ACOs) saved more than $535 million for Medicare last year, after other savings in 2021. That happens through real improvements in patient health, such as better diabetes control and blood pressure screenings that cut back hospitalizations and emergency room visits, said Sean Cavanaugh, chief policy officer for Aledade.
“The data clearly show that ACOs grounded in advanced primary care can deliver better care at lower cost, Cavanaugh said. “But that approach is under threat from consolidation and anticompetitive forces. And let's be clear, the evidence is overwhelming, hospital mergers are steadily increasing, horizontal consolidation leads to higher prices, vertical consolidation leads to higher prices. And there's no clear evidence that consolidation leads to higher quality.”
Instead, provider concentration leads to large health systems demanding higher prices from health plans, Cavanaugh said.
In the hospitals
Hospitals and their more than 6 million workers remain cornerstones of communities, delivering 3.5 million babies and providing emergency care for 123 million people in 2022, said Ashley Thompson, senior vice president for public policy analysis and development of the American Hospital Association.
Hospital leaders are working to comply with price transparency rules that went into effect two years ago. AHA strongly opposes legislation that would lead to additional site-neutral payment cuts and threaten access to patient care, Thompson said.
“There is nothing neutral about site-neutral policies,” she said, with hospitals often handling older, sicker patients with complex medical positions. Likewise, AHA opposes changes that would expand new or existing physician-owned hospitals, Thompson said.
Prescription drugs
For prescription drugs, pharmacy benefit managers (PBMs) administer prescription drug plans for more than 275 million Americans. It is concerning that Congress would consider legislation that would “limit choice by dictating terms to the market, taking away flexibility that is needed for drug costs, keeping health coverage affordable and helping patients stay on their meds,” said Kristin Bass, chief policy and external affairs officer for the Pharmaceutical Care Management Association (PCMA), the PBM industry trade group.
The House subcommittee agenda listed 17 pieces of legislation involving health care, including prescription drugs and PBMs. None of those bills would address drug prices, but would stack the deck in favor of drug makers in negotiating price rebates, Bass said.
“We have to be cognizant of what happens when one side in a negotiation gets confidential information about their competitors negotiated rates, it only leads to higher costs,” Bass said. “Instead, we encourage the subcommittee to address the actual cause of the affordability challenge, the price set by the drug company and the rampant patent abuses that have blocked competition.”
Paying for treatment
Considering serious illness, patients get two forms of bad news: a diagnosis and huge medical bills, said Brian Connell, executive director for federal affairs for the Leukemia and Lymphoma Society. A leukemia diagnosis costs an average of $800,000 in treatment costs the first year, he said.
Costs that patients don’t bear through deductibles and co-pays often go back to consumers and public insurance programs, Connell said. Then, insurance companies and public officials invent new ways to shift costs back to patients.
“We see higher deductibles additional noncovered care, increased coinsurance, rising premiums, more red tape, stricter eligibility criteria for insurance, the list goes on,” Connell said. “And this is why patients need a bold action to make sure that the system is sustainable for patients today and into the future.”
Market competition
Employers paying for health benefits have noticed rising health care costs and marketplace failures in competition, said Ilyse Schuman, senior vice president for health policy for the American Benefits Council (ABC). The group represents more than 220 of the world’s largest corporations dealing with employee benefit issues, and they want to see honest billing and price transparency.
ABC strongly supports site-neutral payment for treatment because it appears hospitals buy physician offices, rebrand them as outpatient departments, then collect higher payments granted to hospitals over physicians, Schuman said.
It’s clear hospitals are an essential component of U.S. health care, especially during the COVID-19 pandemic. But it appears hospitals are losing money due to investment losses, not increased labor and supply costs, Schuman said.
Federal help needed
Consolidation is leading to higher prices for patients, but there are federal policies that would help, said Loren Adler, fellow and associate director of the USC-Brookings Initiative for Health Policy in the Economic Studies Program of the Brookings Institution.
Medicare rates are intended to reflect costs of providing services for an efficient provider.
“As such, Medicare should not be paying more for the same exact service when it's delivered in a hospital outpatient department, rather than a physician's office, provided that the physician's office setting is safe and clinically effective for most patients,” Adler said. Right now, lobbyists are the only ones opposing that concept, he added.
Price transparency and site neutral payment are necessary, and they go together. Adler used the example of a level two nerve injection that costs $256 in a doctor’s office or $741 in a physician practice that was converted to a hospital outpatient department.
“This payment disparity not only increases costs for beneficiaries and taxpayers, but encourages hospitals to buy up physician practices, leading to market consolidation and increased health care costs that spill over to the commercial market as well,” Adler said. “Small efforts have been made to move towards site neutral payments, but more work is needed.”
Administrator speaks
Before the second panel, representatives spent almost 2 ½ hours questioning Chiquita Brooks-LaSure, administrator for the U.S. Centers for Medicare & Medicaid Services (CMS), making her first appearance before the panel.
She outlined various CMS efforts toward the same objectives as the subcommittee.
“We are committed to building on the work that we have done to address rising healthcare costs in a way that helps us advance health equity, expand access, improve health outcomes and increased transparency,” Brooks-LaSure said.
Questions covered a number of topics, including Medicare coverage and availability of Leqembi (lecanemab-irmb), which the U.S. Food and Drug Administration approved this year to treat Alzheimer’s disease. The federal leaders acknowledged a number of audience members wearing purple to show support for the Alzheimer’s Association.
